[ad_1]
Living in the US poses a major threat to a person’s health, and for people between the ages of 25 and 44, the threat is worse, research has found.
About three million deaths are recorded in the US annually, but the nation’s mortality rate is far higher than that of its peers. Researchers calculate a gap between the US and other nations that equals 25 percent of American deaths.
The crisis is most acute for Millennials aged 25 to 44. The gap for this demographic in particular is a whopping 62 percent of deaths.
Millennials span two age groups, according to CDC standards, with one part being 25 to 34 and the other 35 to 44. Their combined annual risk of death falls between 148 and 237 per 100,000 people.
Before 2010, health and societal trends for millennials were moving in a positive direction. Cancer death rates were falling with the advent of groundbreaking specialized care, homicides had plummeted, deaths from heart disease were on the decline and fewer young people were smoking.
But the new decade marked a stark reversal, brought on by the steadily worsening opioid epidemic and a range of other persistent factors, including suicide, homicide, traffic accidents, and metabolic diseases such as diabetes and high blood pressure.
‘We began to see rises in morbidity and mortality because of obesity and, of course, the persistence of firearms,’ Dr Georges Benjamin, who has served as Executive Director of the American Public Health Association since 2002, told the Daily Mail.
‘The cardiovascular disease mortality kind of plateaued for a couple of years, [a decline in deaths due to] cancer kind of plateaued a little bit. And so we started seeing increases in morbidity and mortality pre-pandemic.’

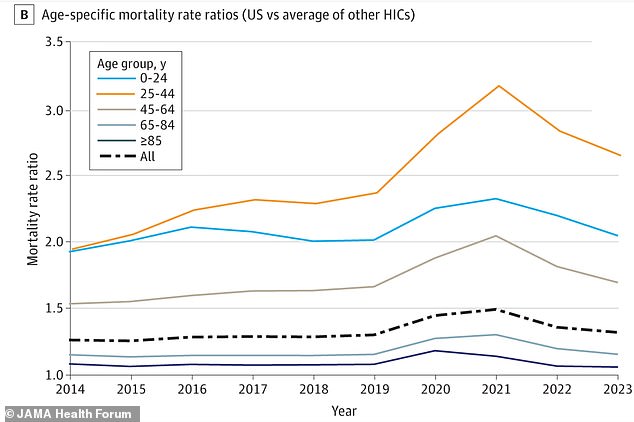
The mortality rate ratio shows how much more likely an American is to die than a person in another high income country. In 2023, US adults aged 25 to 44 were 2.6 times more likely to die than their international peers
Researchers behind a new study on excess deaths found that the pandemic caused a spike in Covid deaths while also amplifying fatalities from overdoses, suicide, accidents and homicide among young adults.
Excess deaths refer to deaths above the number that would be expected if the US had the same mortality rates as other wealthy nations.
A coalition of researchers from Harvard University, the University of Minnesota, Boston University and Hunter College found that a 25- to 44-year-old in the US is 2.6 times more likely to die than a person of the same age in other wealthy countries, such as Australia, Canada, New Zealand, Norway, France, Germany, Spain and others.
‘By 2023, American early adults’ chance of dying was 70 percent higher than it would have been had the lifesaving trends of the early 2000s continued,’ they said.
The exact causes are unclear, but likely drivers include pandemic-era job loss, which exacerbated rising rates of what health researchers call deaths of despair driven by increased substance use and sustained depression that hit young adults hardest.
‘This age group experienced hardships during Covid that are difficult to bounce back from,’ they said.
To measure excess deaths, the team used publicly available (through Human Mortality Database) death records from January 1980 to December 2023 from the US and 21 wealthy peer nations.
The team found 62 percent of deaths in the Millennial group are excess deaths, and observed the gap between the US and other countries is far larger than for any other American age group.

For millennials, nearly two out of three deaths are considered ‘excess’ (stock)
From 1980 to 2023, there were nearly 14.7 million excess deaths in the US.
Excess deaths among millennials spiked during the pandemic and accelerated a pre-existing negative trend where mortality rates from overdoses, suicide and heart disease had already been rising in previous years.
Millennials have been the generation most affected by the opioid epidemic in the US, experiencing the largest share of fatal overdoses compared to other age groups.
According to public health nonprofits Trust for America’s Health and the Well Being Trust, Millennial opioid overdose deaths surged over 500 percent from 1999 to 2017.
During the same period, synthetic opioid death rates increased by 6,000 percent.
Millennials also make up the demographic most likely to be obese, which drastically raises the risk of acquiring a range of disorders from diabetes and heart disease to certain cancers.
Obesity is a significant issue across all age groups, but CDC data reveals that rates climb sharply through early and middle adulthood.
With an obesity rate of 46.4 percent, Americans aged 30 to 39 have the highest prevalence of any age group.
The variety of rising death causes – from accidents to chronic diseases – points to a deep, systemic failure, the research team said.

Nationwide, America has a life expectancy of 77.5 years, according to the latest estimates from the CDC
The millennial generation has faced unique economic hardships and societal challenges, leaving them disillusioned and financially insecure.
‘These economic and health inequities are likely to further increase with cuts to the country’s social safety net, including to programs such as Medicaid, to pay for tax cuts for high earners,’ said the team behind the latest research, published in JAMA Health Forum.
‘Technological advancements may lead to widening income inequality if stable jobs are replaced by AI.’
Dr Benjamin predicted that the US is likely to lag behind fellow wealthy countries for years.
‘Not only are we going to get, in my view, an increased gap between us and the other industrialized nations, but our numbers are going to get worse.
[ad_2]
This article was originally published by a www.dailymail.co.uk . Read the Original article here. .